Consent is not the last word
Stay with me. This might be a bit bumpy. Let’s have a deep conversation about consent. And by consent, I mean consent in a health care context. Consent for treatment or for privacy decisions.
I recently watched an interview with Elizabeth Gilbert and Marie Forleo. In talking about her book, City of Girls, Elizabeth said something along the lines of:
“Consent is important AND it’s not the last word when it comes to female sexuality. There is also desire.”
“Consent sometimes sounds like a passive waiting for someone to come and say what they want to do with your body and you give or don’t give your consent. But desire is when you choose what you want and go after it.”
As a health lawyer, that got me thinking about consent in a health care context.
For recipients of health care services, “patients”, consent is important AND it is not the last word when it comes to patient experience, engagement and empowerment. There is also desire.
What if we take our health care conversations beyond consent to treatment or consent to sharing health information – and we listen to and talk about what patients desire in their treatment? What if we don’t stop at consent when discussing privacy – but invite desire into our understanding of how patients want their information shared or not shared.
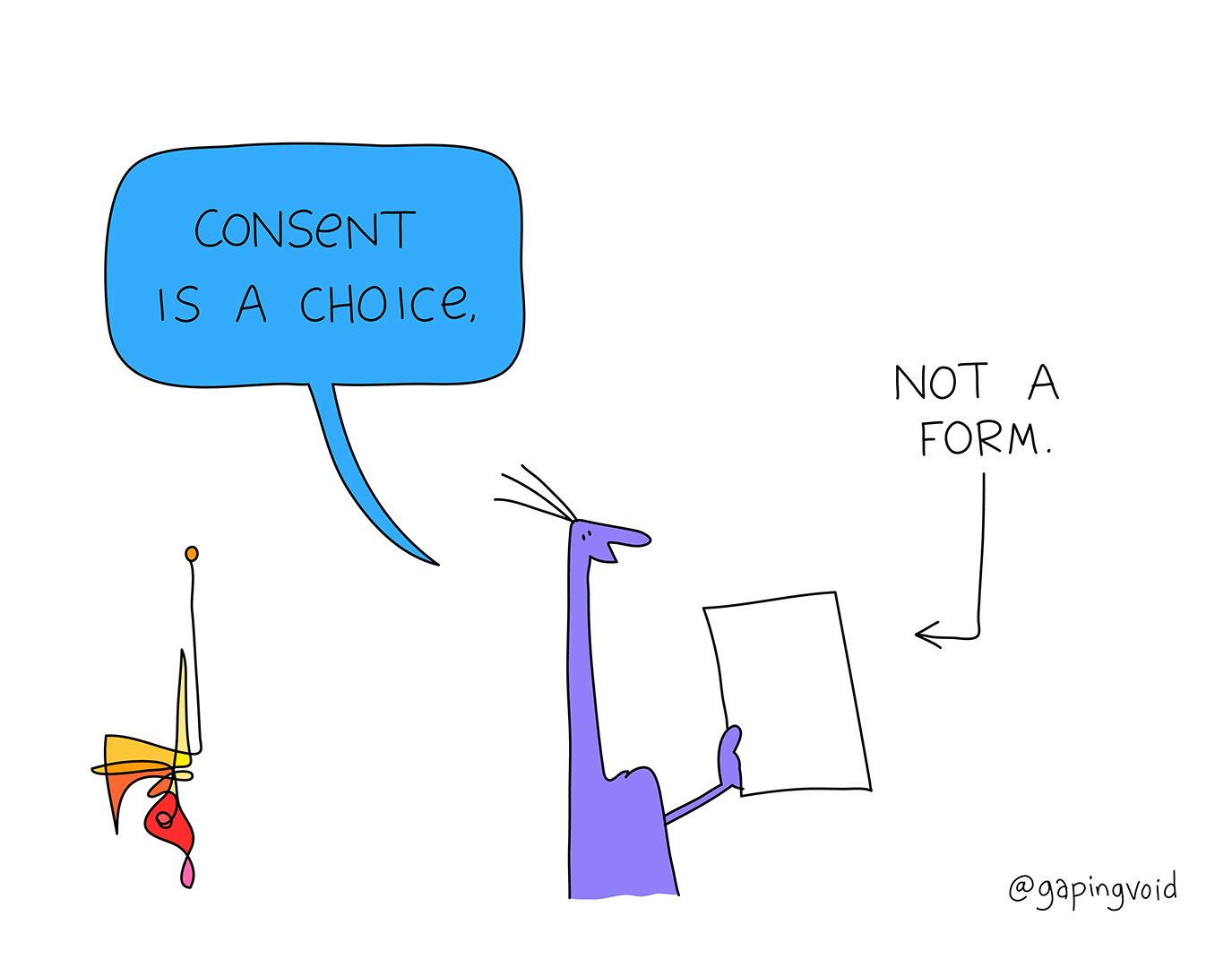
Instead of “consent” – we should talk about choice and desire.
What do patients want?
What choices does a patient have?
How do patients want to feel?
What does a patient want to have happen?
What outcomes does a patient want?
What experiences does the patient desire?
What questions do patients ask (especially in the time before we tell them what is going to happen to them)?
What if we let patients drive the process? What would be different?
To apply Elizabeth Gilbert’s philosophy to the health care context, if we only ever teach consent – we miss the perspective of the patient-driven experience of their own health.
Without desire – patients are not fully themselves and are not able to bring their full perspective and needs to their care experience.
Of course, we must not forget about consent. But let’s make sure that our processes and approach to consent is not about “getting patients to sign our forms”.
When we have the “consent” talk – it is often focused on the health care provider’s or organization’s needs.
When we have a choice or desire talk – it would be focused on what the patient wants.